Final yr practical GENERAL MEDICINE.(1601006136)
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome."
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE:
A 65 year old female with fever,pain abdomen and loose stools.
Chief Complaints :
-fever,
pain abdomen,
vomiting & loose stools since 1 week -
burning micturition since 4 days.
History of presenting illness:
The patient was apparently asymptomatic 1 week back and then developed
-Fever: high grade, intermittent, associated with chills & rigors, relieved with medication
-Lower Abdominal pain : sudden in onset, continuous dull aching/cramping, aggravated with food intake
-vomiting 2-3 episodes/day: non bilious, non projectile, watery with food particles
-Loose stools multiple episodes in large volume watery, no tenesmus, no mucous or blood in stools.
-History of burning micturition since 4 days : high coloured urine, no hematuria
Past history:
History of similar compliant two months back which were relieved on medication.
History of diabetes type-2 since 10years and on regular medication
History of hypertension since 10years and on regular medication
No history of epilepsy/asthma/siezures.
Treatment history:
Diabetes -metformin 500mg+idalgliptin 500mg
Hypertension - telmisartan-40mg
Personal history:
Diet: mixed
Appetite: decreased
Bowel movements :irregular
Bladder : incontinenece with burning micturition.
No known allergies
No addictions
Family history: Not significant
General examination:
Patient is conscious, coherent and cooperative.
Well oriented to time place and person, moderately built,Well nourished
Pallor : present,Icterus - absent,Cyanosis -absent,Koilonychia -absent,Clubbing - absent,Lymphadenopathy - absent,
Edema : facial puffiness present
Vitals:
Temperature: 98.5°c afebrile
BP: 120/80 mm hg
Pulse: 110/ min
Respiratory rate :26/min
SpO2 :96% at room air
Systemic examination:
ABDOMEN
-Inspection:
Shape- distended ,Flanks full
Umblicus: inverted
Movements with respiration- equal in all quadrants.
Skin over abdomen: multiple vertical and horizontal striae
-Palpation :
Tenderness - diffuse mainly right illac fossa
Liver impalpable
Gall bladder impalpable
Spleen impalpable
-Percussion:
Shifting dullness- not present
Fluid thrill not present
-Auscultation
Bowel sound heard
Other system examination
CVS-S1 , S2 normal
Apical impulse 5th intercostal space 2cm later to midclavicular line.
No murmurs
Respiratory system-Normal vesicular breathsounds,Bronchial breath sounds heard,Trachea midline
CNS
Cranial nerve examination : normal
Reflexes : normal
CHEST XRAY
RENAL FUNCTION TEST
COMPLETE URINE EXAMINATION (CUE)
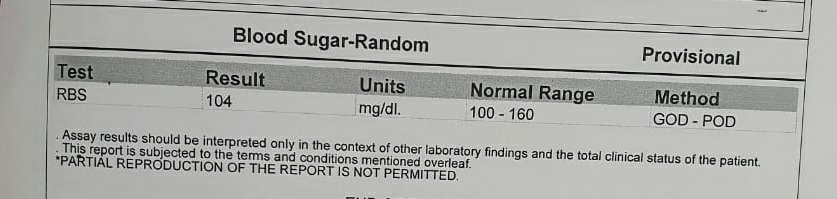
FASTING BLOOD SUGAR(FBS)
USG REPORT
RENAL FUNCTION TEST recent
CUE- 2nd Time
HbA1c
IMPRESSIONS
Renal function tests
Increased serum creatinine levels
Decreased leucocytes
Urine examination:
Increased pus cells in urine
Ultrasound examination
Single cyst in upper lobe of kidney(incidental finding)
provisional Diagnosis:
Acute gastroenteritis with renal cyst.