A 60 YEAR OLD MALE WITH IATROGENIC CUSHING SYNDROME
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome."
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 60 year old man, farmer by occupation, residing at Nalgonda presented to the casualty at 2pm with the
CHIEF COMPLAINTS of
Dyspnea at rest since 10 days
Cough since 10 days
Fever 2 days back
HISTORY OF PRESENT ILLNESS
He was apparently asymptomatic 10 back and then he developed left sided chest pain 10 days back lasting for 30 minutes following which he developed
Dyspnea at rest since the past 10 days along with orthopnea and PND
He also complaints of cough with scanty mucoid expectoration, especially at night time
He gives a history of one episode of low grade fever 2 days back
PAST ILLNESS:-
Since the past 20 years - he started experiencing multiple joint pains.
First involving his right wrist joint followed by right elbow joint following which he developed pains in his left wrist joint and left elbow joint, later he developed pain at his cervical joint following which he also developed pain in his bilateral MCP and PIP as well as DIP joint. He gradually developed lower back ache and bilateral knee joint pains as well.
Everyday morning after getting up he experiences morning stiffness in all his joints so much so that he finds it difficulty to move which lasts for around 15 minutes which would gets relieved on movement.
He later on developed eczematous lesions, hyperpigmneted scaly itchy lesions over his limbs.
He visited a local hospital and consumed NSAIDs and steroids.
10 years back- history of fall from bike but no injury sustained
2 years back - history of hemetemesis for which he paid a visit to Osmania govt hospital where he received 2 blood transfusions and Upper GI endoscopy was done which was normal.
1.5 years back- history of on and off pedal edema and abdominal distension which gets relieved on medications taken from a local hospital ( not documented)
7 months back he presented to us with the complaints of
- Dyspnea since the past 1 year which increased 10 days prior to presentation
- Associated with palpitations
-Left lower limb swelling following glass prick 3 months back with active pus discharge for which he was getting wound dressing and treatment done from a local RMP. At our hospital, wound cultures isolated pseudomonas for which we treated him with Amikacin for 8 days. And we diagnosed him with Iatrogenic cushings syndrome and RA.
PERSONAL HISTORY:-
He is an occasional alcoholic, he occasionally consumes toddy.
He has been smoking about 1 pack of beedis per day since the past 20 years.
ON EXAMINATION:-
On presentation : Patient is conscious, coherent and cooperative and examined in a well lit room.
He is an obese individual with flexion at the PIP joints of his both right and left hand and even toe fingers
Healed ulcer present on his left leg
Vitals -
PR - 89 bpm
Bp - 130/80mmhg
RR - 25cpm
Spo2 - maintaining at 89 % on Room air
Afebrile
No raised JVP
Cvs -
Apex beat at 6th ICS at MCL S1,S2+
Lungs -
Bilateral inspiratory crepts in all Lung fields
Expiratory wheeze in bilateral IAA,ISA
Per Abdomen-
Distended
Non tender
Bowel sounds +
CNS - NAD
We got his 2decho done ( video not available), showed EF 30% with global hypokinesia and dilated LA and LV
INVESTIGATIONS
1.HFREF with EF 30%
2. ? Acute exacerbation of COPD
3. Iatrogenic cushings syndrome
4. Rheumatoid arthritis with eczematous Cutaneous lesions
TREATMENT:-
02/11/21
1) NEB WITH DUOLIN--8TH HOURLY
BUDECORT--12TH HOURLY
2) TAB.PREDISOLONE 15 MG PO/OD
D1 3)TAB.AUGMENTIN 625 MG PO/BD
4) SYP. ASCORYL 10 ML PO/BD
5) TAB. ULTRACET 1/2 tab QID
6) TAB. PCM 500 MG PO/TID
7) MONITOR VITALS 4th HOURLY
8) REVIEW SOS
9) INJ. LASIX 40 MG IV/BD
10) TAB. ECOSPIRIN AV (75/20) MG PO/HS
11) TAB.TELMA 40 MG PO/OD
03/11/21
C/o 1) SOB REDUCED
2) CHEST PAIN+
Treatment:-
1) NEB WITH DUOLIN--8TH HOURLY
BUDECORT--12TH HOURLY
2) TAB.PREDISOLONE 15 MG PO/OD
D2 3)Inj.AUGMENTIN 1.2 Gm IV/BD
4) SYP. ASCORYL 10 ML PO/BD
5) TAB. ULTRACET 1/2 tab QID
6) TAB. PCM 500 MG PO/TID
7) MONITOR VITALS 4th HOURLY
8) REVIEW SOS
9) INJ. LASIX 40 MG IV/BD
10) TAB. ECOSPIRIN AV (75/20) MG PO/OD
11) TAB. ALDACTONE 25 MG PO/OD
12) BIPAP INTERMITTENTLY
13) INJ. HYDROCORTISONE 100 MG IV/OD
14) SYP. DUPHALAC 20 ML HS
04/11/21
C/O 1) CHEST PAIN ON COUGHING
2) CONSTIPATION SONCE 4DAYS
TREATMENT
1) NEB WITH DUOLIN--1resp INH 6THHOURLY
BUDECORT--1 RESP INH 8TH HOURLY
2) TAB.PREDISOLONE 15 MG PO/OD
D3 3)Inj.AUGMENTIN 1.2 Gm IV/BD
4) SYP. ASCORYL 10 ML PO/BD
5) TAB. ULTRACET 1/2 tab QID
6) TAB. PCM 500 MG PO/TID
7) MONITOR VITALS 4th HOURLY
8) REVIEW SOS
9) INJ. LASIX 40 MG IV/BD
10) TAB. ECOSPIRIN AV (75/20) MG PO/OD
11) TAB. ALDACTONE 25 MG PO/OD
12) BIPAP INTERMITTENTLY
13) INJ. HYDROCORTISONE 100 MG IV/OD
14) SYP. DUPHALAC 15ML PO/OD
15) INJ.PANTOP 40MG IV /OD
05/11/21
1) NEB WITH DUOLIN--1resp INH 6THHOURLY
BUDECORT--1 RESP INH 8TH HOURLY
2) TAB.PREDISOLONE 15 MG PO/OD
D3 3)Inj.AUGMENTIN 1.2 Gm IV/BD
4) SYP. ASCORYL 10 ML PO/BD
5) TAB. ULTRACET 1/2 tab QID
6) TAB. PCM 500 MG PO/TID
7) MONITOR VITALS 4th HOURLY
8) REVIEW SOS
9) INJ. LASIX 40 MG IV/BD
10) TAB. ECOSPIRIN AV (75/20) MG PO/OD
11) TAB. ALDACTONE 25 MG PO/OD
06/11/21
SOAP notes
S- SOB reduced
O-
Pt is c/c/c
BP-130/70 mm hg
PR-85 bpm
RR-18 cpm
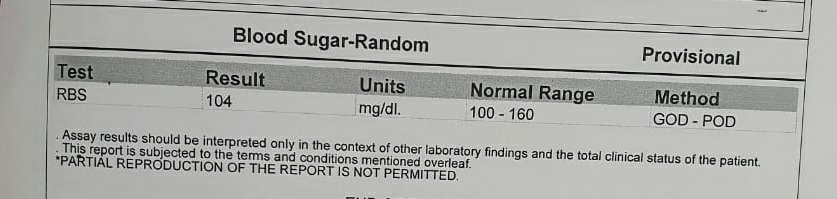
GRBS-104
SPO2:97% on room air
CVS: S1 S2+
RS: BAE+, B/L diffuse rhochi +
P/A: soft, non tender
A-
HFrEF -LVEF 30%
With acute exacerbation of COPD
With k/c/o Iatrogenic cushings syndrome
? RA vasculitis
P-
INJ HYDROCORTISONE 100MG IV TID
T.AZITHROMYCIN 500 MG OD
INJ LASIX 40MG IV BD
INJ. PANTOP 40mg IV OD
INJ. AUGMENTIN 1.2 GN IV BD
NEB DUOLIN 1 RESP INH 6TH HRLY
NEB BUDECORT 1 RESP INH 8TH HRLY
T. PREDNISOLONE 15MG PO OD
T.ULTRACET 1/2 TAB QID
T. ECOSPIRIN AV (75/20) MG PO OD
T ALDACTONE 25MG PO OD
T PCM 500 MG PO SOS
SYP ASCORIL 10ML PO TID
SYP DUPHALAL 15ML PO BD
SOAP WATER ENEMA PR STAT
BO, PR, SPO2,TEMP, CHARTING 4TH HRLY
GRBS 12TH HRLY
BIPAP INTERMITTENTLY.
Date-08/11/2021
SOAP notes
S- SOB reduced
O-
Pt is c/c/c
BP-130/70 mm hg
PR-114 bpm
RR-22 cpm
GRBS-106
SPO2:96% on room air
CVS: S1 S2+
RS: BAE+, B/L diffuse rhochi +
P/A: soft, non tender
A-
HFrEF -EF 30%
With acute exacerbation of COPD
With k/c/o Iatrogenic cushings syndrome
? RA vasculitis
? Hansens disease
P-
D3 --T.AZITHROMYCIN 500 MG OD
TAB. LASIX 40MG IV BD
TAB. PANTOP 40mg IV OD
D7--INJ. AUGMENTIN 1.25 GM IV BD
NEB DUOLIN 1 RESP INH P/N BD
NEB BUDECORT 1 RESP P/N BD
T. PREDNISOLONE 15MG PO OD
T.ULTRACET 1/2 TAB QID
T. ECOSPIRIN AV (75/20) MG PO OD
T ALDACTONE 25MG PO OD
T PCM 650 MG PO SOS
SYP ASCORIL 10ML PO TID
SYP DUPHALAC 15ML PO BD
LIQUID PARAFFIN FOR L/A BD
FUCIDIC CREAM FOR L/A BD
BO, PR, SPO2,TEMP, CHARTING 4TH HRLY
GRBS 12TH HRLY
BIPAP INTERMITTENTLY
--4TH HOURLY